ACNE
Acne will usually go away on its own, but there are treatments than can help clear acne more quickly
Acne is a very common condition, which affects more than 90% of Australian adolescents.
What is Acne?
Acne is a very common skin condition. It causes spots and painful bumps on the skin. It’s most noticeable on the face, but can also appear on the back, shoulders and buttocks.
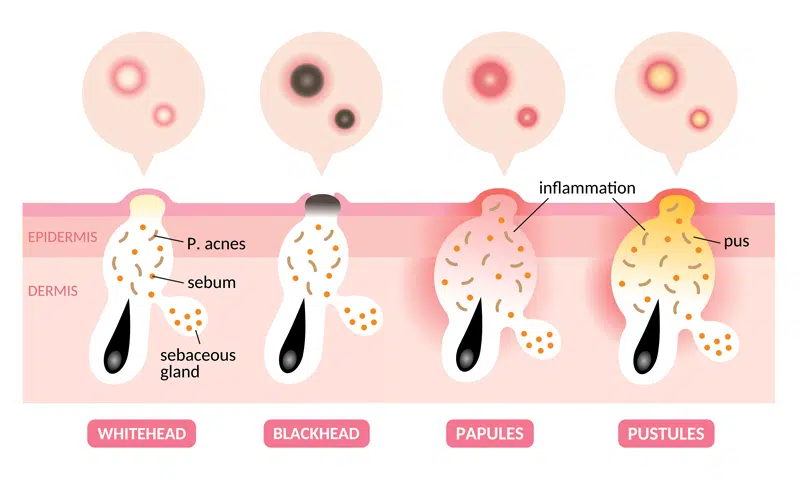
There are four main factors that are involved in the development of acne:
- Abnormal growth of skin cells in the hair follicles causing a plug
- Increased sweat production within sebaceous follicles (sweat glands)
- Proliferation of micro-organisms (Bacteria) in the retained sweat
- Inflammation
Acne Treatment
Acne can be:
· Mild, Moderate or Severe.
Moderate to severe acne has the potential to cause permanent scarring.
There is a strong genetic element in many patients. All acne has an inflammatory basis. Acne has been divided into 4 grades. Whilst it usually may take a few years to resolve on its own, the negative effects that it has on self-esteem, mood and psychological status are significant.
Grade 1

Grade 2

Grade 3

Grade 4

The treatment differs depending on:
- Grade of acne
- Age of the patient
- Other medical conditions
- Social circumstances of the patient
- Age
- Gender
- And many other factors.
The most common treatment includes:
- Appropriate skin care
- Gentle cleansers
- Benzoic acid wash
- Gentle moisturiser with active
When should I see my doctor?
Acne is a medical condition so the smartest thing you can do is seek medical advice, especially if your breakouts are large and painful and/or stopping you from doing the things you love. As Acne is a medical condition it a good idea to have it treated by a medical professional rather than a beauty therapist. Your doctor can assess how bad your acne is and discuss the options with you. Don’t be afraid to tell your doctor how your acne affects your life and how it makes you feel. Some of the treatments your doctor may recommend:
- Topical antibiotics in combination with skin care
- Oral antibiotics may be needed for more severe acne, there are different types and must be tailored to each patient
- Hormonal medications – for example oral contraceptive pill and others
- Diet and lifestyle modification plays an important role – there are more and more studies linking lifestyle to skin conditions including acne
- Light therapy has been shown to be beneficial in some acne – it has to be used with caution especially if a patient is on some acne medications.
- Specialist dermatologist may need to be involved especially when acne is severe
- Psychological and social effects of acne must be considered and referral may also be needed
- Treatment of the associated medical conditions for example PCOS.
The most common reason for treatment failure is insufficient duration of therapy.
Successful treatments require months of therapy and good communication between the doctor and patient and their family. The treatment must be tailored to each person for best results. New treatment options are emerging all the time so speak to your doctor about what is appropriate for you.
REFERENCES
- Kurt Gebauer. Acne in adolescents. Australian Family physician VOL.46, NO.12, DECEMBER 2017
- Marks R, Plunkett A, Merlin K, Jenner N. Atlas of common skin diseases in Australia. Melbourne: epartment of Dermatology, St Vincents Hospital, 1999.
- Koo J. The psychosocial impact of acne: Patients’ perceptions. J Am Acad Dermatol 1995;32(5 Pt 3):S26–30.
- Goldberg JL, Dabade TS, Davis SA, Feldman SR, Krowchuk DP, Fleischer AB. Changing age of acne vulgaris visits: Another sign of earlier puberty? Pediatr Dermatol 2011;28(6):645–48.
- Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol 2013;168(3):474–85.
- Layton AM. Acne scarring – Reviewing the need for early treatment of acne. J Dermatol Treat 2000;11:3–6.
- Kucharska A, Szmurło A, Sińska B. Significance of diet in treated and untreated acne vulgaris. Postepy Dermatol Alergol 2016;33(2):81–86.
- Romańska-Gocka K, Wońniak M, Kaczmarek-Skamira E, Zegarska B. The possible role of diet in the pathogenesis of adult female acne. Postepy Dermatol Alergol 2016;33(6):416–20.
- Berson DS, Shalita AR. The treatment of acne: The role of combination therapies. J Am Acad Dermatol 1995;32(5 Pt 3) S31–41.